Chapter 1 : Initial Assessment & Management
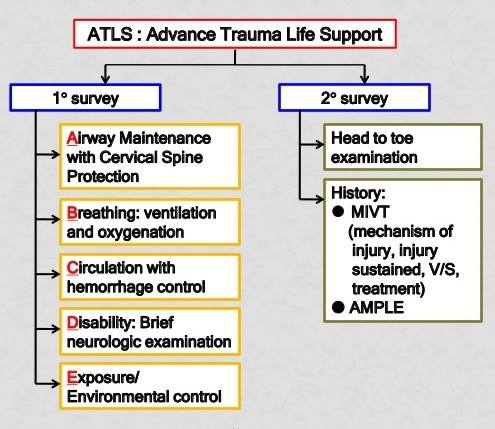
1. Primary survey:
A – Airway + Restriction of cervical spine motion
B – Breathing + Ventilation
C – Circulation + Hemorrhage Control
D – Disability
E – Exposure & Environment control
Adjuncts to primary survey:
a. pulse oximetry/capnopgraphy
b. ABG
c. urinary catheter
d. gastric catheter for decompression e xray (CXR and pelvic cray)
f. FAST/ extended – FAST (eFAST) scan
g. ECG * transurethral catheter contraindict in suspected urethral injury. How to suspect? – blood at urethral meatus – perineal ecchymosis/ swelling
2. Secondary survey
(i) History : A.M.P.L.E. history
A – Allergies
M- Medications
P- past illness/pregnancy
L- last meal
E- events/ environment related to injuries
(ii) Head – to – toe examinations
Adjuncts to secondary survery: specific diagnostic test
Chapter 2 : Airway Management and Ventilation
1. Objective sign of airway obstruction
(a) agitated (suggesting hypoxia)
(b) obtunded (suggesting hypercarbia)
(c) cyanosis
(d) retraction/ use of accessory muscle
(e) abnormal sounds/ noisy breathing
(f) abusive
2. Signs of laryngeal trauma:
hoarseness of voice
subcutaneous emphysema
palpable fracture
3. Objective sign of inadequate ventilation
(a) Asymmetrical chest rise
(b) Decrease/ absent of breath sound
(c) Use of capnography in intubated patient to check ventilation
4. Predicting difficult airway management:
– C- spine injury
– Severe arthritis of C-spine
– Significant maxilofacial/ mandibular trauma
– Limited mouth opening
– Obesity
– Anatomical variation
– Paediatric patient
5. L.E.M.O.N assessment of difficult airway:
L – look externally
E – Evaluate 3-2-2 rule
3 FB – in between incisor’s teeth
2 FB – from hyoid bone to chin
2 FB – from thyroid notch to floor of mouth
M – Mallapati’s score
O – obstruction
N – neck mobility
6. Airway maintainance technique:
(I) Head tilt – chin lift
(ii) Jaw thrust
(iii) nasopharyngeal airway – contraindicated in cribiform plate fracture
(iv) oropharyngeal airway
(v) extraglottic/supraglottic device (LMA, laryngeal tube airway, multilumen esophageal airway)
7. Definitive airway:
(a) orotracheal tube
(b) nasotracheal tube
(c) surgical airway ( cricothyroidectomy, tracheostomy)
8. Criteria establishing for definitive airway
(a) inability to maintain patent airway with impending or potential airway compromise
(b) inability to maintain adequate oxygenation / presence of apnea
(c) obstunded/combasive resulting from cerebral hypoperfusion
(d) obstunded indicating presence of head injury (GCS less or equal 8 or sustained seizure.
Chapter 3 : Shock
Initial Management of Hemorrhagic Shock
1 . Follow ABCDE
2. Obtain vascular access:
minimum of 18 gauge caliber
short large peripheral IV line is preferred (Poiseuille’s law: The rate of flow is proportional to the fourth power of the radius of the cannula and inversely related to it’s length)
3. Initiating fluid theraphy:
1L bolus of crystalloid (warm) for adult ; 20mls/kg for paediatric (< 40kg)
assess pt respond to fluid:
(a) rapid responder
(b) transient responder
(c) minimal or no response
balancing goal of organ perfusion + tissue oxygenation + avoidance of rebleeding (permissive hypotension)
4. Prevention of hypothermia
5. Prevention of coagulopathy
Role of tranexamic acid within 3 hours of injury ( 1st dose given for 10min then 1g over 8 hours)
*massive transfusion
Definition: > 10 units of Packed Cells within 1st 24 hours of admission OR > 4units of Packed Cells transfused over 1 hour
administration of Packed Cells, FFP, Plt in balanced ratio (1:1:1) may improve survical (damage control resuscitation)
*special consideration
1. Advanced age :
– deficit receptor response to cathecholamines
– cardiac compliance reduce with age
– artherosclerotic vasscular disease make vital organ more sensitive in slight reduction in blood flow
– reduced pulmonary compliance, reduce diffusion cpacity + generalised weakness of respiratory muscles limits ability to cope with increase demand of gas exchanges
2. Athelete :
– have remarkable ability to compensate blood loss, may not manifest the usual response to hypovolaemia
3. Pregnancy – hypovolaemia might be reflected in decrease in fetal perfusion
4. Pacemaker – unable to response to blood loss as expected (HR remain as device’s set rate)
Credits : https://www.facebook.com/afiq.fahimy/posts/2085465794893839?_rdc=1&_rdr