AIM : prevention of secondary brain injury (from hypotension, hypoxemia, increased ICP etc.) since neuronal death is irreversible.
| Concussion | Physiological dysfunction without anatomical or radiological abnormality (physiological dysfunction is the first step towards cell death, but is reversible if no further insult occurs) Usually recovers in 2-3 hours |
| Contusion | Small haematoma <1cm |
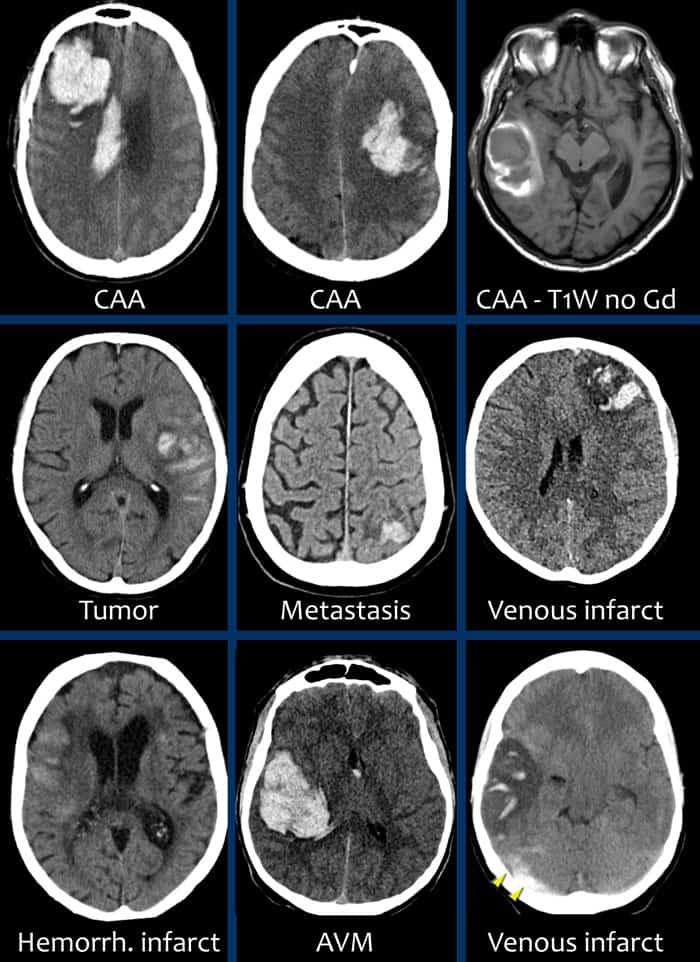
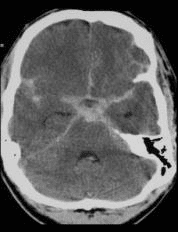
Intracranial Haemorrhage
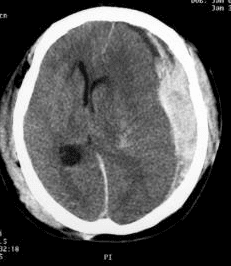
Extradural Haemorrhage (EDH)
Pathology: result from laceration of middle meningeal artery due to temporal bone # – can cause rapid neurological deterioration – if > 1cm in width or have positive clinical symptoms -> urgent surgical evacuation
Classically presents with ‘lucid interval’ which precedes rapid deterioration
20% of patients with EDH are alert and well; brain is minimally damaged, thus drainage gives good results
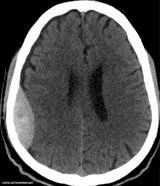
Subdural Haemorrhage (SDH)
Acute SDH : high-speed acceleration / deceleration trauma which shears small bridging (emissary) veins
– More severe than EDH (usually due to nature of injury that causes SDH to occur – associated with higher impact, thus brain has other injuries) – (i.e. shaken baby syndrome, in which similar shearing forces classically cause intra- and pre-retinal haemorrhages)
– Pathology: underlying brain damage in addition to expanding SOL
– Removal of blood does not solve brain damage -> poorer results
Chronic SDH : present in elderly and alcoholics days to weeks after initial HI – can cause focal neurological deficits, AMS, metabolic abnormalities and/or seizures
– If symptomatic = stop anticoagulants / antiplatelets, reverse effect by FPP, PT complex, factor Vii, platelet transfusion, observe and monitor, once resolve = burr-hole drainage + subdural drain placement
Traumatic Subarachnoid Haemorrhage (SAH)
– Usually only small amount of blood -> conservative tx sufficient
Intraparenchymal Haemorrhage (IPH)
Any shape, size, location
– If large haematoma, will require evacuation
Diffuse Axonal Injury
– A major causes of unconsciousness and persistent vegetative state after head trauma
– If severe, will see punctate haemorrhages at the grey-white border
– Arises from injury that causes rotational and shearing forces (high impact injury) – rapid acceleration and deceleration of brain in the intracranial cavity against relatively fixed points of attachment at the falx and tentorium (e.g. RTA, falls, assaults, shaken baby syndrome)
– Maximal effects at corpus callosum and brainstem
Cerebral oedema (3 types)
1. Hypoxic / Cytotoxic (cellular)
– Decreased blood supply (oxygenation) -> loss of function of Na-K pump as ATP decreases -> increased intracellular sodium -> cellular swelling
– Conventionally thought to be resistant to any known medical treatment
2. Interstitial
– Impaired absorption of CSF -> increases in transependymal CSF flow -> acute hydrocephalus
– Also not responsive to steroid administration, and its response to osmotherapy is debatable
3. Vasogenic
– Breakdown of blood-brain barrier -> proteins enter interstitial space -> oedema
– Seen in TBI, neoplasms, and inflammatory conditions
– This oedema subtype is responsive to both steroid administration and osmotherapy